CONDITIONS
Diabetes
Insulin Resistance and Diabetes
Insulin acts like a key to let blood sugar into cells for use as energy.
Invisible changes in the body begin long before a person is diagnosed with type 2 diabetes. That’s both bad news (no symptoms mean you won’t know you have it) and good news (you can prevent or delay it if you’re at risk). One of the most important unseen changes? Insulin resistance.
Insulin, Blood Sugar, and Type 2 Diabetes Insulin is a key player in developing type 2 diabetes. This vital hormone—you can’t survive without it—regulates blood sugar (glucose) in the body, a very complicated process.
Here are the high points:
- The food you eat is broken down into blood sugar.
- Blood sugar enters your bloodstream, which signals the pancreas to release insulin.
- Insulin helps blood sugar enter the body’s cells so it can be used for energy.
- Insulin also signals the liver to store blood sugar for later use.
- Blood sugar enters cells, and levels in the bloodstream decrease, signaling insulin to decrease too.
- Lower insulin levels alert the liver to release stored blood sugar so energy is always available, even if you haven’t eaten for a while.
That’s when everything works smoothly. But this finely tuned system can quickly get out of whack, as follows:
- A lot of blood sugar enters the bloodstream.
- The pancreas pumps out more insulin to get blood sugar into cells.
- Over time, cells stop responding to all that insulin—they’ve become insulin resistant.
- The pancreas keeps making more insulin to try to make cells respond.
- Eventually, the pancreas can’t keep up, and blood sugar keeps rising.
Lots of blood sugar in the bloodstream is very damaging to the body and needs to be moved into cells as soon as possible. There’s lots of insulin, too, telling the liver and muscles to store blood sugar. When they’re full, the liver sends the excess blood sugar to fat cells to be stored as body fat. Yep, weight gain. And what’s more serious, the stage is set for prediabetes and type 2 diabetes.
Prediabetes
What Is Prediabetes?
Prediabetes is a serious health condition where blood sugar levels are higher than normal, but not high enough yet to be diagnosed as type 2 diabetes. Approximately 88 million American adults—more than 1 in 3—have prediabetes. Of those with prediabetes, more than 84% don’t know they have it. Prediabetes puts you at increased risk of developing type 2 diabetes, heart disease, and stroke.
The good news is that if you have prediabetes, the CDC-led National Diabetes Prevention Program can help you make lifestyle changes to prevent or delay type 2 diabetes and other serious health problems.
What Causes Prediabetes?
Insulin is a hormone made by your pancreas that acts like a key to let blood sugar into cells for use as energy. If you have prediabetes, the cells in your body don’t respond normally to insulin. Your pancreas makes more insulin to try to get cells to respond. Eventually your pancreas can’t keep up, and your blood sugar rises, setting the stage for prediabetes—and type 2 diabetes down the road.
Signs & Symptoms
You can have prediabetes for years but have no clear symptoms, so it often goes undetected until serious health problems such as type 2 diabetes show up. It’s important to talk to your doctor about getting your blood sugar tested if you have any of the risk factors for prediabetes, which include:
-
- Being overweight
- Being 45 years or older
- Having a parent, brother, or sister with type 2 diabetes
- Being physically active less than 3 times a week
- Ever having gestational diabetes (diabetes during pregnancy) or giving birth to a baby who weighed more than 9 pounds
- Having polycystic ovary syndrome
Race and ethnicity are also a factor: African Americans, Hispanic/Latino Americans, American Indians, Pacific Islanders, and some Asian Americans are at higher risk.
Simple Blood Sugar Test
You can get a simple blood sugar test to find out if you have prediabetes. Ask your doctor if you should be tested.
OBESITY
Data & statistics
Public health surveillance is the ongoing systematic collection, analysis, and interpretation of outcome-specific data for use in planning, interpretation, and evaluation of public health practice. The latest statistics, surveillance systems, state indicator reports and maps related to obesity are provided.
Obesity is a common, serious, and costly disease
- The prevalence of obesity was 42.4% in 2017~2018. [Read CDC National Center for Health Statistics (NCHS) data brief]
- From 1999–2000 through 2017–2018, the prevalence of obesity increased from 30.5% to 42.4%, and the prevalence of severe obesity increased from 4.7% to 9.2%.
- Obesity-related conditions include heart disease, stroke, type 2 diabetes and certain types of cancer that are some of the leading causes of preventable, premature death.
- The estimated annual medical cost of obesity in the United States was $147 billion in 2008 US dollars; the medical cost for people who have obesity was $1,429 higher than those of normal weight.
- Obesity affects some groups more than others
- Non-Hispanic Black adults (49.6%) had the highest age-adjusted prevalence of obesity, followed by Hispanic adults (44.8%), non-Hispanic White adults (42.2%) and non-Hispanic Asian adults (17.4%).
- The prevalence of obesity was 40.0% among adults aged 20 to 39 years, 44.8% among adults aged 40 to 59 years, and 42.8% among adults aged 60 and older.
HYPERTENSION
Facts About Hypertension in the United States
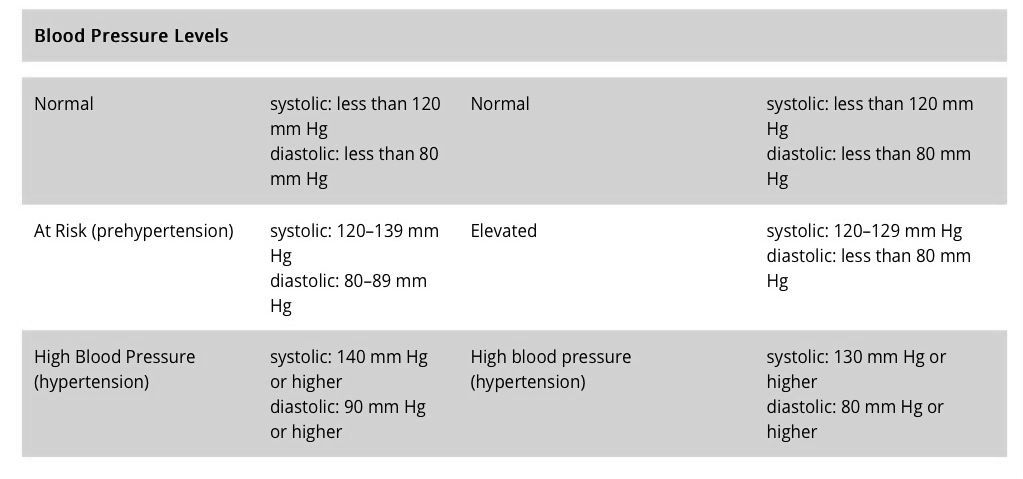
In 2017, the American College of Cardiology and the American Heart Association published new guidelines for hypertension management and defined high hypertension as a blood pressure at or above 130/80 mm Hg. Stage 2 hypertension is defined as a blood pressure at or above 140/90 mm Hg.
Prevent High Blood pressure:
By living a healthy lifestyle, you can help keep your blood pressure in a healthy range. Preventing high blood pressure, which is also called hypertension, can lower your risk for heart disease and stroke. Practice the following healthy living habits:
Eat a Healthy Diet
Choose healthy meal and snack options to help you avoid high blood pressure and its complications. Be sure to eat plenty of fresh fruits and vegetables.
Talk with your health care team about eating a variety of foods rich in potassium, fiber, and protein and lower in salt (sodium) and saturated fat. For many people, making these healthy changes can help keep blood pressure low and protect against heart disease and stroke.
The DASH (Dietary Approaches to Stop Hypertension) eating plan is a healthy diet plan with a proven record of helping people lower their blood pressure.
Keep Yourself at a Healthy Weight
Having overweight or obesity increases your risk for high blood pressure. To determine whether your weight is in a healthy range, doctors often calculate your body mass index (BMI). If you know your weight and height, you can calculate your BMI at CDC’s Assessing Your Weight website. Doctors sometimes also use waist and hip measurements to assess body fat.
Talk with your health care team about ways to reach a healthy weight, including choosing healthy foods and getting regular physical activity.
Be Physically Active
Physical activity can help keep you at a healthy weight and lower your blood pressure. The Physical Activity Guidelines for Americans external icon recommends that adults get at least 2 hours and 30 minutes of moderate-intensity exercise, such as brisk walking or bicycling, every week. That’s about 30 minutes a day, 5 days a week. Children and adolescents should get 1 hour of physical activity every day.
Do Not Smoke
Smoking raises your blood pressure and puts you at higher risk for heart attack and stroke. If you do not smoke, do not start. If you do smoke, quitting will lower your risk for heart disease. Your doctor can suggest ways to help you quit.
Limit How Much Alcohol You Drink
Do not drink too much alcohol, which can raise your blood pressure. Men should have no more than 2 alcoholic drinks per day, and women should have no more than 1 alcoholic drink per day. Visit the CDC’s Alcohol and Public Health website for more information.
Get Enough Sleep
Getting enough sleep is important to your overall health, and enough sleep is part of keeping your heart and blood vessels healthy. Not getting enough sleep on a regular basis is linked to an increased risk of heart disease, high blood pressure, and stroke.
LIPID DISORDER
The term “lipid disorder” covers a range of conditions that can cause abnormal levels of lipids, or fats, in the blood.
These fats include low-density lipoproteins (LDLs), also known as “bad” cholesterol, and fatty acids called triglycerides. High-density lipoproteins (HDLs), known as “good” cholesterol, are also present in the blood.
This article will look at the symptoms of lipid disorders, their causes, and what treatments are available, including lifestyle changes people can make to prevent or reduce high cholesterol.
What is a lipid disorder?
A lipid disorder will typically increase levels of LDLs, triglycerides, or both. HDLs are known as good cholesterol because they help to transport bad cholesterol out of the body.
A buildup of LDLs and triglycerides can cause fatty materials to accumulate in the body’s tissues, including in the arteries. This can have serious consequences for cardiovascular health and increase the risk of problems such as heart disease.
The American Academy for Family Physicians say 1 in 3 adults in the United States have high levels of LDL cholesterol. This is why healthcare professionals advise people to cut down on fatty foods and increase their HDL levels to help remove the bad cholesterol
Symptoms of lipid disorder
It is important to point out that, most of the time, a person will have no symptoms of a lipid disorder until they experience a significant health problem, such as a stroke or heart attack.
However, the following symptoms have been occasionally observed in some people with very high lipid levels:
- yellowish, fatty bumps or yellow creases on the skin, formed by an accumulation of fatty deposits around tendons and joints (xanthomas)
- white arcs around the cornea of the eye (arcus senilis), which sometimes occur in younger people with high cholesterol
- raised, yellow lumps at the inner corners of the eyes (xanthelasma)
Lipid disorders, such as high cholesterol, are common in the U.S.
A healthy diet and lifestyle can help to reduce cholesterol, especially if combined with medication.
People who are worried about a family history of high cholesterol, or any symptoms associated with lipid disorders, should talk with a healthcare professional.
ARTHRITIS
Factors that Increase Risk of Getting Arthritis
Arthritis is common; in fact, about 1 in 4 US adults have arthritis. Some behaviors and characteristics, called risk factors, increase an adult’s likelihood of getting some types of arthritis or making it worse. You can control some risk factors, and others you cannot. You can decrease your risk of getting arthritis or making arthritis worse by changing the risk factors you can control.
Learn about known risk factors and what you can do to lower your risk of developing arthritis.
Risk Factors You Can Control
Modifiable risk factors are risk factors that you can control. Making lifestyle changes can decrease your risk of getting some types of arthritis or making arthritis worse.
Overweight and Obesity
People who are overweight or obese are more likely to get knee osteoarthritis than people who are not overweight. Excess weight can also make knee osteoarthritis worse. Extra weight puts more stress on joints, particularly weight-bearing joints like the hips and knees.
- What you can do: Maintain a healthy weight. Healthy eating and physical activity can help you lose weight and stay at a healthy weight. Learn how you can eat healthy and safely exercise with arthritis.
Infection
Many microbial agents, like bacteria and viruses, can infect joints and potentially cause the development of some types of arthritis.
- What you can do: See your doctor right away if your joints are swollen, warm, or red. It might be an infection.
Joint Injuries
Joint injury or overuse such as knee bending and repetitive stress can damage a joint and contribute to the development of osteoarthritis in that joint.
- What you can do: Protect your joints from injuries by doing special exercises for those joints. Visit the OA Action Alliance website for exercises to prevent knee injuries
Occupation
Occupations that involve repetitive knee bending and squatting are associated with osteoarthritis of the knee.
What you can do:
Make sure your worksite is free of fall hazards and has the space, equipment, and tools that fit your physical ability and limitations. Learn about ergonomics and musculoskeletal disorders from CDC’s National Institute for Occupational Safety and Health (NIOSH).
Smoking
Cigarette smoking increases a person’s risk of developing rheumatoid arthritis (RA) and can make the disease worse. It can also cause other medical problems. Smoking can also make it more difficult to stay physically active, which is an important part of managing RA and other types of arthritis.
COPD
What is COPD?
Chronic obstructive pulmonary disease, or COPD, refers to a group of diseases that cause airflow blockage and breathing-related problems. It includes emphysema and chronic bronchitis.
Who has COPD?
Chronic lower respiratory disease, primarily COPD, was the third leading cause of death in the United States in 2014.1 Almost 15.7 million Americans (6.4%) reported that they have been diagnosed with COPD.2 More than 50% of adults with low pulmonary function were not aware that they had COPD,3 so the actual number may be higher.
The following groups were more likely to report COPD in 2013,
- People aged 65 to 74 years and ≥75 years.
- American Indians/Alaska Natives and multiracial non-Hispanics.
- People who were unemployed, retired, or unable to work.
- People with less than a high school education.
- People who were divorced, widowed, or separated.
- Current or former smokers.
- People with a history of asthma.